
AFWG shall not bear any responsibility for any content on such sites. Any link to a third-party site does not constitute an endorsement of the third party, their site or services. AFWG also makes no warranties as to the content of such sites.
Would you like to continue?
Professor Jeremy Day
Wellcome Trust Intermediate Fellow
Head, CNS & HIV Infections Research Group
Oxford University Clinical Research Unit
Ho Chi Minh City, Vietnam
Cryptococcal meningitis
The global incidence of HIV-associated cryptococcal meningitis is estimated to be around 223,100 cases per year, resulting in 181,000 deaths.1 Few drugs are available for treatment and many have poor efficacy presented with toxicities. Combination antifungal therapy is the recommended treatment for cryptococcal meningitis.
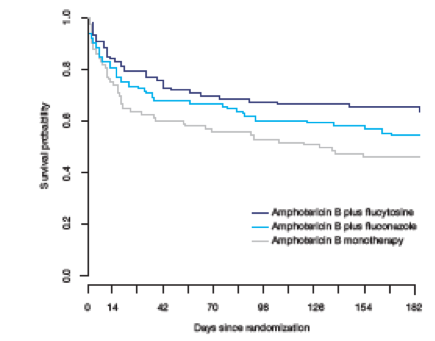
Previous data from a randomized controlled trial conducted in Vietnam showed that amphotericin B plus flucytosine was associated with improved survival compared with amphotericin B alone (15 vs 25 deaths at day 14; hazard ratio [HR]: 0.57; p=0.08; and 30 vs 44 deaths at day 70; HR: 0.61; unadjusted p=0.04) (Figure 1).2 This combination also resulted in faster yeast clearance from cerebral spinal fluid (CSF) than amphotericin B monotherapy or amphotericin B combined with fluconazole 800 mg/day. Rates of adverse events were similar across both groups. Access to both amphotericin B and flucytosine has the potential to reduce the mortality of HIV-associated cryptococcal meningitis. In contrast, combining fluconazole with amphotericin B for 2 weeks offered no survival benefit compared with 4 weeks of amphotericin B monotherapy. The rate of CSF fungal clearance is associated with the survival outcome; this measure has utility in evaluating novel antifungal treatment regimens, but trials powered to important clinical endpoints are still needed. Recently, the Antifungal Combinations for Treatment of Cryptococcal Meningitis in Africa (ACTA) trial has been published, which has demonstrated the key role that flucytosine can play in delivering more efficacious oral treatment and allowing shortened durations of amphotericin therapy.3
Figure 1. Kaplan-Meier survival estimates according to treatment groups2
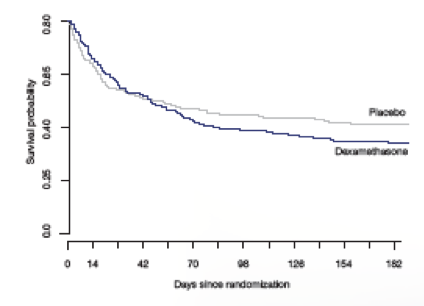
Professor Day also presented the results of the CryptoDex trial of adjunctive treatment with dexamethasone in HIV associated cryptococcal meningitis.4 In this trial, patients were randomized to dexamethasone or placebo for 6 weeks, in addition to best available antifungal treatment.4 The mortality rate was 57% vs 49% by 6 months, respectively (HR: 1.18; p=0.20) (Figure 2). Patients in the dexamethasone group also experienced higher risk of death or disability compared with placebo with 13% vs 25% having pre-specified good outcomes (odds ratio [OR]: 0.42; p<0.001). The use of dexamethasone is harmful and should not be given as an adjunctive treatment.
Figure 2. Kaplan-Meier survival estimates during the 6 months follow-up4
Talaromycosis (penicilliosis)
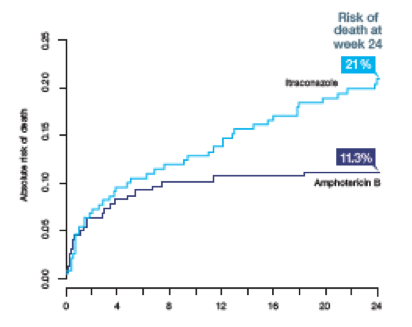
Talaromycosis infection is a common cause of HIV-related deaths in Asia. The American and British treatment guidelines recommend initial treatment with amphotericin B followed by itraconazole.5,6 This regimen is based on a non-comparative trial conducted in Thailand that showed 97% treatment response in 74 patients.7 A non-inferiority trial comparing amphotericin B and itraconazole demonstrated lower risk of death with the former at week 24 (11.3% vs 21%; p=0.006) (Figure 3).8 Amphotericin B also resulted in significantly faster fungal clearance and clinical resolution compared with itraconazole. However, more patients experienced anemia and electrolyte disturbances. Based on the outcomes of this trial, amphotericin B must be considered the treatment of choice for talaromycosis.
Figure 3. Estimated risk of death at week 24 in patients receiving itraconazole vs amphotericin B for HIV-associated talaromycosis8
Clinical pearls
Highlights of the Medical Mycology Training Network Conference, December 1–3, 2017, Ho Chi Minh City, Vietnam
References