
AFWG shall not bear any responsibility for any content on such sites. Any link to a third-party site does not constitute an endorsement of the third party, their site or services. AFWG also makes no warranties as to the content of such sites.
Would you like to continue?
Ms Ratna Mohd Tap and Dr Fairuz Amran
Mycology Laboratory
Infectious Diseases Research Centre
Institute for Medical Research
Kuala Lumpur, Malaysia
Fereydounia khargensis represents a new lineage in the order Urocystales, subphylum Ustilaginomycotina. It was first discovered in Iran in 20141; in 2016, RM Tap et al reported 2 invasive infections caused by F. khargensis in immunocompromised patients in Malaysia, which are discussed below.2
The first case of F. khargensis was from an HIV-positive patient. He was admitted because of episodes of fever associated with chills and rigors for 2 weeks. The patient was initially treated with amphotericin B, but the clinical condition did not improve. Antifungal treatment was changed to itraconazole and he was discharged upon improvement.
The second case was a hepatitis B carrier with hypertension, diabetes mellitus and end-stage renal failure on continuous ambulatory peritoneal dialysis (CAPD). He was admitted because of a dislodged distal connector of his Tenckhoff catheter caused by a fall in the toilet. After the incident, the dislodged connector was reconnected to the Tenckhoff catheter and used for CAPD. Fluconazole was started following yeast growth from the peritoneal fluid. The clinical condition of the patient improved after fluconazole treatment.
Both cases grew yeast-like colonies. Figures 1 and 2 show the macro- and microscopic examinations. Results from API 20C AUX and VITEK 2 identification system were Cryptococcus neoformans (98% probability) and Cryptococcus laurentii (89% probability), respectively. Internal transcribed spacer (ITS) and D1/D2 region in large subunit (LSU) of rRNA gene were amplified using universal primers and sequenced. Both F. khargensis isolates matched 99.7% (ITS) and 100.0% (LSU) to the reference strain, IBRC-M 30116.
Figure 1. F. khargensis colonies on Sabouraud dextrose agar (SDA) after 48 h incubation at 30°C presented as cream-colored colonies, dry and wrinkled (a). However, after 72 h of incubation, the colonies started producing melanin-like pigmentation, which turned even darker after 120 h (b).
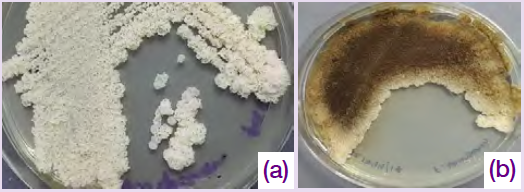
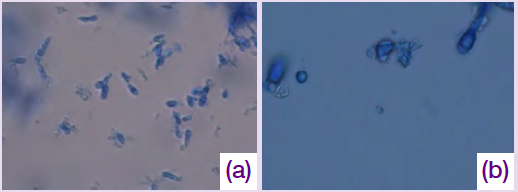
Figure 2. Elongated and irregular shape of F. khargensis yeast cells from 48 h SDA plate. The length of the cells ranged from 5.63 to 18.34 μm. Magnification at x40 (a) and x100 (b).
In vitro susceptibility testing showed that itraconazole and voriconazole have good activity against the yeast with minimum inhibitory concentration (MIC) ranging from 0.032 to 2.000 µg/mL, but MIC was slightly higher for fluconazole (8.000 µg/mL). On the other hand, both isolates showed resistance to amphotericin B, caspofungin and anidulafungin with the MIC more than 32.000 µg/mL.
In summary, F. khargensis is a new and uncommon opportunistic yeast. The incidence of rare fungal pathogens is rapidly increasing due to the expanding population of immunocompromised patients and advanced identification techniques. In this report, low CD4 count (case 1) and complicated medical conditions (case 2) are the risk factors that predisposed the patients to F. khargensis infection. Observation of macroscopic and microscopic characteristics provides clues to their atypical features. Correct identification is crucial and can be made possible by polymerase chain reaction (PCR) sequencing. F. khargensis exhibited resistance to polyenes and echinocandin but was sensitive to azoles.
References