
AFWG shall not bear any responsibility for any content on such sites. Any link to a third-party site does not constitute an endorsement of the third party, their site or services. AFWG also makes no warranties as to the content of such sites.
Would you like to continue?
Dr Atul Patel, MD, FIDSA
Chief Consultant and Director
Infectious Diseases Clinic
Vedanta Institute of Medical Sciences
Ahmedabad, India
A 49-year-old female patient was previously diagnosed with sarcoidosis and interstitial lung disease, and has been receiving steroids for her medical condition over the last 15 years. She previous received empirical anti-tuberculosis treatment but has stopped after a few months due to adverse drug reaction. Pulmonary function test showed severe restriction with diffusion defects. Two-dimensional echocardiography and antinuclear antibody were normal. High-resolution chromatography showed end-stage fibrotic changes in bilateral lung parenchyma with honeycombing, secondary bronchiectasis in bilateral upper and lower lobes.
Clinical presentation
Earlier in June 2017, the patient was admitted to the hospital with fever, worsening respiratory symptoms and peripheral cyanosis. She had a total leukocyte count (TLC) of 16,200 and a galactomannan reading of 1.36. Her bronchoscopy appeared normal. Aspergillus fumigatus was identified in her bronchoalveolar lavage fluid. She was started on itraconazole 200 mg/day but had no clinical response.
The patient went to consult another pulmonologist. Two-dimensional echocardiography showed left ventricular ejection fraction at 55% and right ventricular systolic pressure at 11 mmHg signaling moderate to severe pulmonary hypertension. The patient was tested negative for anti-cyclic citrullinated peptide. Repeat CT scan of the thorax revealed thick-walled cavity with a surrounding halo sign in left lower lobe (Figure 1). Since she was diagnosed with invasive aspergillosis, her antifungal was changed to voriconazole 200 mg BID.
Figure 1. CT scan of the thorax showed thick-walled cavity with a surrounding halo sign in left lower lobe

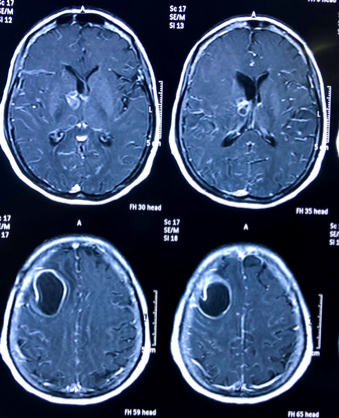
In October 2017, the patient was admitted to the emergency room with fever, headache and an episode of convulsion on the same day. Examination revealed the patient was drowsy but arousable and could follow verbal commands. She had tachycardia and hypoxia but was afebrile. She was anemic with a hemoglobin level of 10.7 g/dL, and TLC was 16,600. She had a pro-brain natriuretic peptide value of 1,419 pg/mL and elevated C-reactive protein of 4.5 mg/L. Her liver enzymes were normal and no abnormalities were detected in her chest X-ray and ultrasound. Neurological reference advised a CSF examination and a magnetic resonance imaging (MRI) of the brain. CSF examination reported the following: glucose 68mg/dL; protein: 105mg/dL; white blood cell count 120/ cmm with 20% neutrophils and 80% lymphocytes. No organism was detected on Gram or Ziehl-Neelsen stain. CSF cryptococcal antigen and CSF GenXpert MTB/RIF assays were negative; CSF adenosine deaminase level was 3.38 and CSF galactomannan test yielded 4.06. The MRI showed an abscess in the left frontal parietal region. Contrasts also showed multiple lesions located at the basal ganglia region (Figure 2). Serum IgG antibodies against toxoplasma was negative.
Figure 2. MRI with contrast showed a large abscess in the left frontoparietal region with multiple lesions located at the left basal ganglia region
Neurophysician suggested anti-tuberculosis therapy (isoniazid, rifampin, ethambutol, and pyrazinamide) with steroids. At this point, an infectious disease consultation was requested. The patient’s history and treatment reviewed two important observations: 1) The patient experienced clinical deterioration with brain involvement after more than 6 weeks on voriconazole. 2) Voriconazole trough level were not measured. The infectious disease physician advised to stop anti-tuberculosis treatment and continued with voriconazole, requested voriconazole trough levels be measured and neurosurgical reference for draining the brain abscess. The patient was started with 2 g ceftriaxone injection every 12 hours and anti-seizure treatment. Direct microscopic examination of the sample from the brain abscess revealed partially acid-fast beaded filaments (Figure 3). Microbiological culture grew Nocardia farcinica, which was confirmed with matrix-assisted laser desorption/ionization time of flight (MALDI-TOF) mass spectrometry. Her voriconazole trough level was 5.72 mg/L. She was given ceftriaxone and trimethoprim/sulfamethoxazole for her nocardia infection and had a clinical response to the antimicrobials.
Figure 3. Direct microscopic examination of the brain abscess sample revealed partially acid-fast beaded filaments
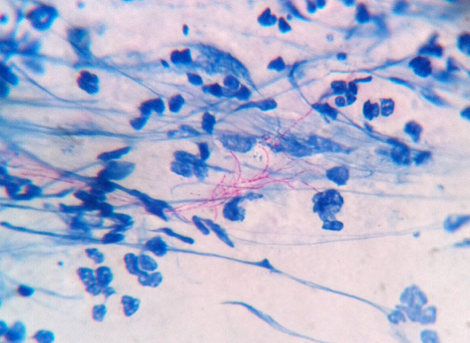
Table 1. Diagnosis performance of galactomannan in CSF according to different cutoffs.1
Parameter | Value (%) with CSF galactomannan ODI cutoff of | |||||
0.5 | 1.0 | 2.0 | 3.0 | 4.0 | 5.0 | |
Sensitivity
| 88.2 | 88.2 | 88.2 | 76.5 | 70.6 | 58.8 |
Specificity
| 96.3 | 96.3 | 96.3 | 96.3 | 96.3 | 96.3 |
Positive predictive value | 93.8 | 93.8 | 93.8 | 92.9 | 92.3 | 90.9 |
Negative predictive value | 92.9 | 92.9 | 92.9 | 86.7 | 83.9 | 78.8 |
CSF, cerebral spinal fluid; ODI, optical density index. | ||||||
Discussion
The first important learning objective from this case was the selection of antifungal agent and dosage for a patient diagnosed with invasive pulmonary aspergillosis (IPA). Itraconazole, initially selected by the pulmonologist of this case, is generally not recommended as a first choice in the management of IPA due to erratic absorption and significant drug-drug interactions with acid-suppressing agents. Voriconazole is a treatment of choice for IPA. Cerebral aspergillosis is a likely possibility in an immunocompromised patient diagnosed with IPA. The second learning point is how one should evaluate disease progression on appropriate antifungal therapy for >6 weeks. This could be due to inadequate voriconazole trough level leading to treatment failure. Clinicians should check voriconazole trough levels in every patient with IFI because it is associated with high mortality. Brain abscess aspiration and microbiologic examination can confirm the diagnosis of CNS aspergillosis. CSF fungal biomarkers, eg, CSF galactomannan and β-D-glucan, are useful in making a diagnosis of CNS fungal infection in a situation where brain aspiration or biopsy is not possible.
Galactomannan detection is one of the microbiological criteria for the diagnosis of cerebral aspergillosis. CSF galactomannan with an optical density index (ODI) cutoff of 0.5 to 2.0 has high specificity and sensitivity (Table 2), and could be used to diagnose cerebral aspergillosis without needing cerebral biopsy.1 β-D-glucan in cerebrospinal fluid is also a useful biomarker for the diagnosis of CNS fungal infections.2
Monitoring trough levels for voriconazole may be important for patients who are not responding optimally or have drug interactions that may decrease voriconazole levels. Although voriconazole resistance is rising globally, lack of response is mostly due to significant drug-drug interactions and the variation in metabolism in patients with CYP2C19 polymorphisms.
Clinical pearls
Highlights of the Medical Mycology Training Network Conference, December 1–3, 2017, Ho Chi Minh City, Vietnam
References